Synthetic opioids represent one of the most pressing public health challenges. In 2023 alone, drug overdoses claimed around 105,000 lives in the U.S.—with opioids responsible for nearly 80,000 of those deaths, or more than three out of every four.
Unlike their natural counterparts derived from opium poppies, synthetic opioids have fundamentally influenced opioid dependence and overdose deaths. They have created new complexities in treatment and recovery. Therefore, understanding these substances is more critical than ever.
In this article, we explore what synthetic opioids are, how they affect the body, and the risks they pose, while examining warning signs of addiction and, most importantly, effective treatment options available today for those struggling with opioid dependence.
What Are Synthetic Opioids?

Synthetic opioids are artificially manufactured drugs that mimic the effects of natural opiates by binding to the same receptors in the brain.
The distinction between synthetic and natural opioids has real-world implications for potency, safety, and treatment approaches. While natural opioids have been used for medicinal purposes for centuries, synthetic variants can be engineered to be far more potent. Consequently, this can lead to increased risks of overdose and dependence.
Synthetic vs. Natural Opioids
Natural opioids, also called opiates, come directly from the opium poppy plant. These include morphine and codeine, which have predictable effects and well-established medical protocols. Semi-synthetic opioids like oxycodone and heroin are chemically modified from natural opioids but retain some connection to their plant origins.
Synthetic opioids, however, are made from scratch using chemical precursors. This manufacturing process allows for variations in molecular structure that can alter potency and effects. The unpredictability of these modifications makes synthetic opioids particularly dangerous.
The table below outlines some of the key differences between synthetic and natural opioids:
| Natural Opioids (i.e.opiates) | Synthetic Opioids | |
| Source | Derived directly from the opium poppy plant (e.g., morphine, codeine) | Man-made in laboratories to mimic or enhance opioid effects (e.g., fentanyl, methadone) |
| Potency | Generally lower potency compared to synthetics | Often far more potent, fentanyl can be 50–100 times stronger than morphine |
| Medical Use | Severe pain relief and cough suppression | Severe pain management, anesthesia, and opioid use disorder treatment |
| Risk of Overdose | Present; lower than synthetic opioids but can increase depending on dose, tolerance level, and other substances used | Extremely high due to exceptional strength, especially with illicit formulations. Major driver of overdose crisis, especially illicit fentanyl and its analogs |
Examples of Synthetic Opioids
Synthetic opioids, other than methadone, include a wide range of substances, from legitimate prescription medications to dangerous street drugs:
Prescription Synthetic Opioids:
- Fentanyl (Duragesic, Actiq, Sublimaze)
- Methadone (Dolophine, Methadose)
- Tramadol (Ultram, ConZip)
- Demerol (Pethidine, Meperidine)
- Dextropropoxyphene (Darvon)
Illicit Synthetic Opioids:
- Illicitly manufactured fentanyl
- Carfentanil
- U-47700 (“Pink” or “Pinky”)
- Acetylfentanyl
- Furanylfentanyl
- MT-45
- AH-7921
Designer Synthetic Opioids:
- Nitazenes (including isotonitazene)
- Benzimidazole opioids
- Novel fentanyl analogs
The sheer number of synthetic variants continues to grow as illegal manufacturing leads to new formulations to evade detection. This constant evolution makes synthetic opioids a moving target for both law enforcement and healthcare providers.
How Synthetic Opioids Work
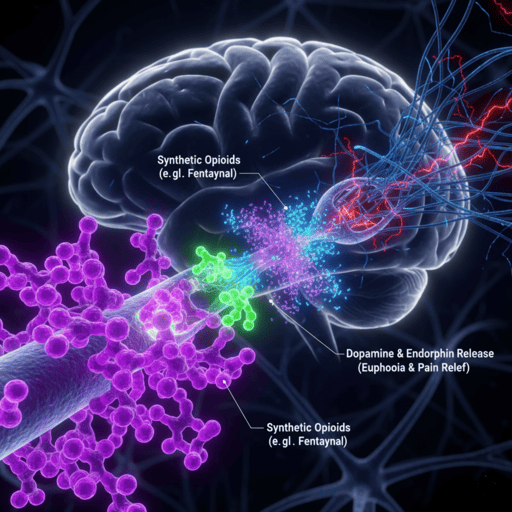
Synthetic opioids bind to opioid receptors throughout the central nervous system, primarily targeting mu-opioid receptors in the brain and spinal cord. When these synthetic substances attach to receptors, they trigger the same neurochemical cascades as natural endorphins, but often with dramatically amplified intensity.
The binding process disrupts normal pain signaling and activates brain reward pathways. This dual action explains why synthetic opioids provide powerful pain relief while simultaneously creating euphoric effects that contribute to their addictive potential.
What makes synthetic opioids particularly concerning is their enhanced potency. Fentanyl, for example, is approximately 50 times more potent than heroin and 100 times more potent than morphine. This extreme potency means that tiny amounts can produce profound effects, making dosing unpredictable and overdoses more likely.
The rapid onset and intense effects of synthetic opioids also accelerate the development of tolerance and physical dependence. Users often find themselves in need of larger doses to achieve the same effects, a dangerous cycle that quickly leads to opioid dependence.
Risks and Dangers of Synthetic Opioids
According to the CDC’s National Center for Health Statistics, approximately 48,422 people in the U.S. lost their lives to overdoses from fentanyl in 2024. Synthetic opioids exacerbate the crisis, creating unprecedented risks that go beyond traditional opioids.
Now, let’s examine these risks and dangers to see how they impact users.
#1. Unpredictable Potency and Composition
Street-manufactured synthetic opioids often contain toxic adulterants or varying concentrations of active ingredients. This unpredictability has turned every use into a potential life-threatening gamble.
Users frequently don’t know what they’re taking or how strong it is. What appears to be heroin might actually contain fentanyl that’s dozens of times more potent. This contamination has led to countless accidental overdoses and deaths among people who thought they were using familiar substances.
#2. Rapid Development of Dependence
Synthetic opioids create physical dependence faster than most other substances. The intense receptor binding and rapid onset mean that regular use quickly leads to neurochemical changes. Users often find themselves dependent after just a few uses, trapped in a cycle they never intended to enter.
The withdrawal symptoms from synthetic opioids can be particularly severe and prolonged. Many people continue using them not for euphoric effects but simply to avoid the crushing discomfort of withdrawal. This creates a vicious cycle in which users feel they have no choice but to continue.
#3. Overdose Risk and Respiratory Depression
The narrow margin between an effective dose and a lethal dose makes synthetic opioids extremely dangerous. Respiratory depression—the slowing or stopping of breathing—can occur rapidly and without warning. Unlike overdoses from other substances, synthetic opioid overdoses often require multiple doses of naloxone (Narcan) to reverse.
Emergency responders report that synthetic opioid overdose symptoms are more difficult to treat and more likely to result in death. The synthetic opioid side effects include not just respiratory depression but also cardiac complications that can prove fatal even when breathing is restored.
Signs You May Have a Synthetic Opioid Problem

Recognizing the signs of synthetic opioid dependence can be challenging, as these substances often create dependence before users realize they have a problem. The rapid onset of physical dependence means that what starts as occasional use can quickly become a daily necessity.
Physical signs often appear first and may include:
- Extreme drowsiness or nodding off at inappropriate times
- Constricted pupils that don’t respond to light changes
- Slowed or irregular breathing patterns
- Frequent flu-like symptoms that improve with drug use
- Unexplained weight loss and poor personal hygiene
- Track marks, bruises, or infections at injection sites
Behavioral changes typically follow as the dependence deepens. Users may become secretive about their activities, lose interest in previously enjoyed activities, or neglect responsibilities at work, school, or home. Financial problems often emerge as the cost of maintaining the habit grows.
One of the most evident warning signs of dependence is the inability to function without the substance. When synthetic opioids are needed just to feel “normal” rather than to achieve a high, it’s a strong indicator that physical dependence has developed—a condition that requires professional treatment.
Treatment Options for Synthetic Opioid Addiction
Traditional approaches to treating synthetic opioid dependence fall short because they don’t address the underlying neurobiological changes these substances create. Most conventional treatments focus on managing withdrawal symptoms rather than repairing the damaged endorphin system.
Medication-assisted treatment (MAT) programs use replacement opioids like methadone or buprenorphine. While these approaches can help stabilize users by providing prescription replacement opioids, they do not address the underlying neurochemical imbalances caused by long-term opioid use.
ANR treatment goes beyond symptom management. Accelerated Neuro-Regulation directly addresses the opioid-induced changes in brain chemistry by modulating the endorphin system back to its pre-dependence state.
The ANR procedure is performed in an ICU setting under sedation, allowing physicians to address withdrawal while patients are asleep and do not feel the uncomfortable withdrawal symptoms.. Unlike traditional detox methods that only detox drugs from the system, ANR actually repairs the neurobiological damage caused by chronic opioid use. Patients typically return to their daily lives within days, free from both cravings and withdrawal symptoms.
Key Takeaways
Synthetic opioids are more potent, unpredictable, and dangerous than their natural counterparts. Due to their potency, there is a higher risk of opioid dependence development and fatal overdose.
Understanding the signs of synthetic opioid dependence is crucial for early intervention. Physical dependence can develop quickly, often before users realize they have a problem. The key is recognizing that dependence is a medical condition, not a personal failure.
Key points to remember:
- Synthetic opioids are far more potent than natural opioids, making overdose more likely
- Physical dependence can develop rapidly, sometimes after just a few uses
- Traditional treatment approaches often substitute one dependence for another
- ANR treatment addresses the neurobiological root causes of dependence
- Recovery is possible with proper medical intervention



